You feel a deep toothache that does not go away. Cold water sends a sharp jolt that lingers, your gums look swollen, or one tooth appears darker than the others. It is easy to assume the worst. However, not every toothache requires a root canal.
The real issue is what’s happening inside the tooth. When the pulp becomes severely inflamed or infected, the damage often cannot be reversed on its own. This is when root canal treatment is necessary.
Catching the signs early makes treatment simpler and more predictable, and may help reduce the broader inflammatory effects untreated dental infections can cause in the body.
Key Takeaway
- Persistent pain and lingering thermal sensitivity are the strongest clinical indicators of irreversible pulp inflammation.
- Swelling, gum abscess, discoloration, or mobility signal infection may have progressed beyond the pulp.
- Early intervention preserves natural teeth and may reduce systemic inflammatory burden.
The 8 Major Signs You May Need a Root Canal
Each symptom below explains what you feel, what is happening biologically, when it becomes serious, and what dentists observe clinically.
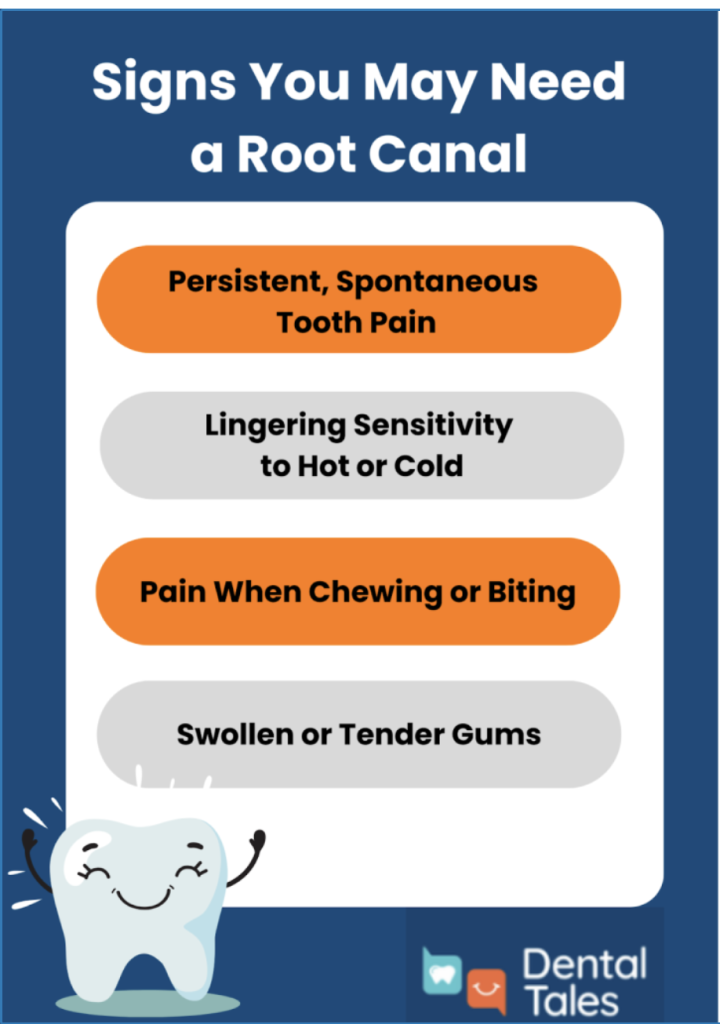
- Persistent, Spontaneous Tooth Pain
What you feel: A throbbing, deep ache that comes and goes without any trigger. The pain might wake you up at night or intensify when you lie down. The pain can occur without chewing or touching the tooth. It may feel like pressure from inside.
When it becomes serious: If the pain persists for more than 48 hours, recurs frequently, or intensifies rather than resolves, the pulp inflammation has likely become irreversible. At this stage, the tissue cannot heal on its own, and the infection will continue to spread if left untreated.
What dentists see clinically: During examination, I often find that the affected tooth is extremely sensitive to percussion (tapping). The X-ray might show a deep cavity approaching the pulp chamber, or sometimes a dark shadow at the root tip, indicating bone loss from infection.
- Lingering Sensitivity to Hot or Cold
What you feel: When you drink something hot or cold, the pain doesn’t fade quickly like it normally would. Instead, it lingers for minutes after you’ve finished, sometimes 10, 15, or even 30 minutes.
The difference between reversible and irreversible pulpitis: If the sensitivity is brief (a few seconds) and the pain is mild, you might have reversible pulpitis; the pulp is irritated but can still heal with proper treatment, like a filling.
But when the pain lingers for minutes, you’re likely dealing with irreversible pulpitis, meaning the pulp tissue is too damaged to recover and will need root canal treatment.
What dentists see clinically: I perform a cold test using a refrigerant spray or ice stick. In cases of irreversible pulpitis, the tooth shows an exaggerated response that takes significantly longer to subside compared to adjacent healthy teeth.
- Pain When Chewing or Biting
What you feel: Sharp pain when you bite down on food or when you release the bite. You might find yourself unconsciously chewing on one side of your mouth to avoid that particular tooth. The discomfort can range from a dull ache to a severe, shooting pain.
When it becomes serious: If the pain continues beyond a few days or worsens progressively, it indicates the infection is spreading.
What dentists see clinically: During percussion testing, even gentle tapping on the tooth with an instrument causes significant discomfort. X-rays often reveal widening of the periodontal ligament space or a dark area at the root tip where the bone is being destroyed by infection.
- Swollen or Tender Gums
What you feel: The gum around a specific tooth becomes puffy, red, and tender to the touch. The area might feel warm and look shiny. Sometimes the swelling is subtle; other times, it’s quite noticeable and may even affect your face’s appearance if it spreads.
When it becomes serious: If the gum swelling spreads to your cheek, under your jaw, or causes difficulty swallowing or breathing, this is a dental emergency requiring immediate care.
What dentists see clinically: I look for localized tenderness and redness in the attached gingiva (the firm gum tissue near the tooth). The area may be painful to touch, and sometimes I can feel fluctuance, a squishy sensation indicating fluid accumulation beneath the surface.
- Gum “Pimple” or Abscess (Fistula)
What you feel: A small, pimple-like bump appears on your gum, usually near the root of a specific tooth. Sometimes it swells up, drains, and then reappears in a recurring cycle. You might not feel much pain because the drainage is actually releasing the built-up pressure.
When it becomes serious: Persistent drainage or recurring swelling requires urgent treatment.
What dentists see clinically: I can trace the fistula tract using a special technique to identify exactly which tooth is causing it. X-rays typically show bone loss around the infected tooth’s root. Interestingly, patients with fistulas often report less pain than those with acute abscesses because the drainage relieves pressure.
- Tooth Discoloration (Grey or Dark Yellow)
What you feel: You might not feel anything at all; discoloration is often painless. Your tooth gradually takes on a grey, dark yellow, or brownish tint compared to neighboring teeth. The change can be subtle at first, becoming more noticeable over months or years.
When it becomes serious: Any noticeable change in tooth color warrants a dental evaluation. Even if you’re not experiencing pain, a dead pulp can still harbor bacteria that may eventually cause infection. Early treatment is simpler and more predictable.
What dentists see clinically: I check the tooth’s vitality using cold tests and electric pulp testers. Discolored teeth typically show no response, confirming pulp necrosis. X-rays help determine if the infection has spread to the surrounding bone. Addressing discolored teeth before infection develops leads to better outcomes.
- Tooth Mobility
What you feel: Your tooth feels slightly loose when you touch it with your tongue or finger. It might shift very subtly when you bite down. This looseness is distinctly different from the natural slight movement all teeth have; this feels wrong, unstable.
When it becomes serious: Any new tooth mobility is a red flag. While some cases of mobility from infection can stabilize after root canal treatment, extensive bone loss may compromise the tooth’s long-term prognosis. Immediate evaluation helps determine if the tooth can be saved.
What dentists see clinically: I measure mobility on a scale from 0 to 3, with higher numbers indicating more severe looseness. X-rays reveal the extent of bone loss. CBCT scans (three-dimensional x-rays) provide even more detailed information about bone destruction and help predict treatment success.
- Cracked or Deeply Decayed Tooth
What you feel: You might notice a rough edge on your tooth, see visible brown or black areas, or feel food getting stuck in the same spot repeatedly. Sometimes you experience intermittent sharp pains when biting at certain angles. Other times, a large portion of your tooth may have already broken off.
When it becomes serious: Any cavity that causes spontaneous pain or sensitivity likely approaches or involves the pulp. Cracks that cause sharp pain when biting in specific directions may extend into the pulp. The sooner these are addressed, the better the chance of saving the tooth with root canal treatment rather than extraction.
What dentists see clinically: I carefully examine the extent of decay and use various techniques to detect cracks, staining, transillumination with bright lights, and high-magnification loupes. Deep cavities often show pulp exposure when I clean out the decay. The location and extent of cracks significantly impact whether the tooth can be saved.
Symptom Severity Guide
Understanding the urgency of your symptoms helps you make informed decisions about seeking care:
| Symptom | Monitor | See Dentist Soon | Urgent |
| Cold sensitivity | Brief, sharp pain lasting seconds | Pain lasting more than 30 seconds | Pain continuing for several minutes |
| Swelling | Slight gum irritation or tenderness | Localized swelling near one tooth | Spreading swelling to cheek/jaw, difficulty swallowing |
| Pain | Occasional discomfort that responds to pain relievers | Persistent pain returning regularly | Severe throbbing pain unrelieved by medication |
| Abscess/bump | – | Small gum bump with drainage | Growing abscess with facial swelling |
| Discoloration | Subtle color change without symptoms | Noticeable darkening | Dark tooth with associated pain or swelling |
While this guide will provide you with the general direction, trust your instincts. If something feels seriously wrong, don’t wait; schedule an appointment immediately. You can also refer to my guide on what a dental emergency is here, so you can always stay informed and take the right steps for your oral health.
Symptom Progression Timeline
Understanding how infections progress helps explain why early intervention matters:
Stage 1: Deep Cavity Forms
Bacteria work their way through tooth enamel and into the softer dentin layer beneath. At this stage, you might notice some sensitivity to sweets or cold, but the tooth usually responds well to a filling.
Stage 2: Bacteria Reach the Pulp
Once bacteria penetrate the pulp chamber, your immune system responds with inflammation. You begin experiencing more persistent sensitivity and occasional spontaneous pain. The pulp tissue is fighting hard but becoming overwhelmed.
Stage 3: Inflammation Increases Pressure
As inflammation intensifies within the rigid walls of your tooth, pressure builds. This is when the characteristic throbbing pain develops. The compressed nerves send constant pain signals, and the discomfort becomes harder to ignore.
Stage 4: Pulp Tissue Dies
Eventually, the infection kills the pulp tissue. Interestingly, this sometimes causes a temporary reduction in pain, leading people to mistakenly believe the problem has been resolved. In reality, the infection is still actively spreading; you just can’t feel it anymore because the nerves are dead.
Stage 5: Abscess Forms
With no living tissue left to contain them, bacteria spread beyond the root tip into the surrounding bone. An abscess develops, a pocket of pus and dead tissue. This may cause swelling, a gum bump, or renewed severe pain.
Stage 6: Bone Loss Begins
Chronic infection progressively destroys the bone supporting your tooth. The longer the infection persists, the more bone loss occurs. Extensive bone loss can compromise the tooth’s long-term stability, even after successful root canal treatment.
Each stage that passes makes treatment more complex and the outcome less predictable. What could have been resolved with a simple filling in Stage 1 becomes a root canal by Stage 3, and may progress to extraction if you wait until Stage 6.
Also learn: How to remove plaque at home
Conclusion
Early detection significantly increases treatment success and reduces complications. Root canal therapy today is highly predictable, safe, and supported by decades of clinical research.
Delaying treatment allows infection to spread deeper into the bone and surrounding tissues, increasing the risk of extraction and more complex procedures.
Preserving your natural tooth helps maintain chewing efficiency, jawbone stability, bite alignment, and long-term oral health. Reducing chronic dental infection may also lower systemic inflammatory burden, which is increasingly linked to metabolic and cardiovascular health.
If symptoms persist, worsen, or recur, timely evaluation is the safest and most cost-effective option.
FAQ Section
- Can a root canal heal on its own?
No. Once pulp tissue becomes irreversibly inflamed or infected, it cannot regenerate. Temporary relief may occur if pressure decreases, but the bacteria remain inside the canal system. Definitive treatment is required to eliminate the infection.
- Does it always hurt?
Not always. Acute infections can be very painful, but chronic infections may cause minimal or no discomfort. Some patients only notice discoloration or a small gum swelling.
- Is extraction better than a root canal?
In most cases, preserving the natural tooth is preferred. Extraction creates a gap that may require an implant, bridge, or partial denture to restore function. Keeping your natural tooth maintains bone density and normal bite mechanics.
- Can infection spread to the body?
Yes. Untreated dental infections can spread locally into facial spaces and, in rare but serious cases, enter the bloodstream. Chronic oral infection has also been associated with elevated inflammatory markers.
- How long can I wait before treatment?
If pain lasts more than 48 hours, sensitivity lingers, or swelling develops, evaluation should not be delayed. Waiting increases the chance of bone loss, abscess formation, and more extensive treatment.